Mirena IUD side effects: the ultimate guide
Mirena (levonorgestrel-releasing intrauterine system or LNG-IUD) is a popular birth control method. It is a hormone-releasing IUD (intrauterine device). While generally safe the use and removal of such devices may be associated with some side effects and risks, which are described in detail in this post.
What is Mirena and how does it work?
Female reproductive system consists of ovaries, fallopian tubes, uterus and genital organs. As hormones are one of the most important factors that control your capability to get pregnant, there are lots of effective hormonal birth control methods.
During menstrual cycle one or more eggs get released from ovaries and move down to uterus through fallopian tubes.
When fertilized the egg starts growing and gets implanted in the uterus.
Therefore uterus is one of the sites where hormonal and other contraceptive methods act.
The innermost lining of the uterus, called the endometrium, is the most critical part of the uterus, as far as the implantation of the foetus is concerned.
During the proliferative phase of the menstrual cycle, the endometrium undergoes a growth spurt where the endothelium, as well as the glands increase both in size and functionality.
That’s where levonorgestrel-releasing intrauterine systems come into the play.
Mirena makes use of a synthetic progestin called levonorgestrel, which is derived from 19-nortestosterone.
It acts locally (e.g. its effects are limited to the endometrium of the uterus - see image below).
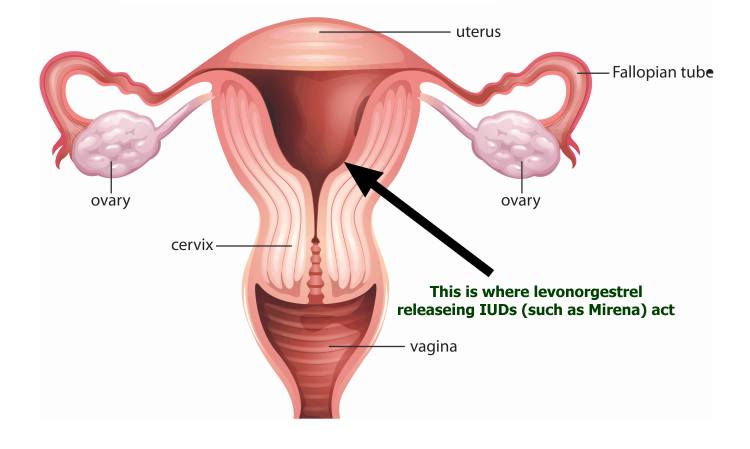
Female reproductive system
Unlike oral contraceptives, Mirena only causes the thinning of the uterus and atrophy of its glands. Also, unlike oral contraceptives, it has minimal effects on ovulation and its effects are long term lasting for years (1).
Mirena is a reversible birth control device and it is made by the Bayers Pharmaceuticals.
This IUD is quite flexible and is implanted inside the uterus.
It is usually used by women who have at least one child.
It is also used by women having heavy menstrual bleeding.
This device was approved by the Food and Drug Administration Authority (FDA) in 2000 and is one of the two hormonal IUDs approved in the United States.
The FDA expanded the Mirena approval in 2009 for treating heavy menstrual bleeding in women using IUD (2).
The device is quite effective in controlling pregnancy for up to 2 years, after which it should be replaced.
Mirena seems to be quite an effective device and is used by more than 150 million women worldwide (3).
The popularity of Mirena is growing in the United States and in 2011 it made up 10.4 percent of the contraceptives prescribed by doctors compared to 1.4 percent in 2002.
You should never try to insert the device by yourself.
It must be inserted by a licensed doctor.
The cost of this device is around $800.
Mirena is more effective than many contraceptives, because once it is inserted, you shouldn’t worry about taking a pill on daily basis.
The effectiveness relies on the perfect use, which means must take the pill on daily basis.
Most oral contraceptives have a failure rate of 30 percent because they aren’t taken effectively.
Mirena failure rate is about 1 percent.
Risks, problems, side effects and complications associated with Mirena
Mirena has an excellent safety profile.
Since it causes only local effects and it only releases the hormones quite slowly, it does not have the similar spectrum of side effects as seen with typical contraceptives.
Still, it is a device containing hormones and like other medicines or devices, it has a number of side effects associated with it.
The side effects associated with the use of Mirena can be divided into two main categories:
- The side effects, risks or complications associated with the use of Mirena
- The side effects, risks or complications associated with the removal of Mirena
Side effects, risks or complications associated with the use of Mirena
Here is the list of side effects or complications associated with the use of this IUD.
Spotting
Typical IUDs, including the copper-T (a copper-based IUD), may cause an increase in the menstrual blood flow. The typical IUDs are known to cause a 50-100% increase in the blood flow during the menstrual cycles (4).
Mirena actually causes a decrease in menstrual blood flow (oligomenorrhea and even amenorrhea), rather than an increase.
While lots of women are happy about it and consider this to be Mirena benefit, sometimes it may be quite troublesome (e.g. due to nonexistent periods - amenorrhea) (5).
The most annoying bleeding related side effect of Mirena is spotting in some women, which is one of the most frequent causes of early discontinuation of this IUD (6).
Pain and cramping
Some women also complain about Mirena associated pain and cramping. There have been several case reports of women experiencing continuous abdominal pain following the insertion of Mirena, which resulted in early removal of the device (7).
However the majority of women (including those who experience a lot of pain during the insertion process) claim that Mirena is a trouble free birth control device.
While Mirena insertion may be associated with some pain, this pain should go away within a few days. If not and/or if you start to suffer from abdominal cramps, you need to go to see your doctor immediately as continuous pain and cramps might be a sign of Mirena expulsion.
Weight gain
Weight gain is one of the most common side effects of Mirena use. If you are conscious about your weight, then Mirena might not be one of the best choices for you. Mirena is a contraceptive and contraceptives usually cause weight gain.
Levonorgestrel in Mirena leads to an increase in the deposition of body fat. While weight gain is considered a general side effect with the use of contraceptives but it is marginally greater with the use of Mirena than with copper T.
In one research a group of 76 women were studied for changes in their body weight following the use of contraceptive devices. The women were divided into two groups based on their method of contraception.
One group used Mirena while the other one used copper-T IUD.
The body weights of these groups were noted at the time of insertion and after 12 months.
The two groups did not differ much in their body weight initially.
However, both the groups experienced gain in weight at the end of 12 months.
The Mirena group experienced an average 3 kg gain in weight compared to the copper T group in which the average gain in weight was only 1.5 kg.
Moreover, this gain in weight was mainly due to increase in fat deposition (8).
Headache
A headache is one of the commonly reported side effects of Levonorgestrel (9).
But unlike other contraceptive devices, the chances of a headache or a migraine with the use of Mirena are significantly lower.
Only a few of Mirena users have dropped out because of headaches.
Moreover, migraine, with or without aura, is generally a contraindication for contraceptive pill use.
However, Mirena seems not to worsen migraines and females having migraine, with or without aura, can safely use it without the risk of aggravating the symptoms (10).
Psychological issues
Mirena IUD is known to cause a number of psychological issues. The real mechanism behind this effect of Minera is still poorly understood. In fact, the psychological disturbance causes by Mirena is one of the main reasons for the discontinuation of Mirena use.
As much as 3% of the females going for Mirena removal blame the depression caused by Mirena use to the prime reason for their decision for removing the device. This is in comparison of the 0% incidence of depression seen with the use of copper T (11).
In addition to depression, the use of Mirena is also associated with other psychological disturbances like anxiety, mood swings, and behavioral changes (12).
Pregnancy
Mirena is one of the most effective methods of sterilization with the lowest failure rates. Still, there are 0.1% chance of Mirena failing and the women getting pregnant as a result (13).
The biggest problem with the pregnancy acquired while an IUD is in place is the risk of ectopic pregnancy. Ectopic pregnancy is a condition in which the foetus gets implanted in a place other than the uterus. It can be the fallopian tubes, pelvis or some other place. Ectopic pregnancy can lead to a lot of complications like acute abdominal bleeding, bursting of fallopian tubes, and a shock-like condition.
There is a small risk of ectopic pregnancies associated with Mirena use. The incidence of Mirena IUD associated ectopic pregnancies is 1 in 1000 pregnancies in 5 years (10).
Perforation
This is another serious complication associated with IUD use.
Although Mirena is made of inert material it can still trigger an inflammatory response in the uterus. As a result, the device erodes through the walls of the uterus and penetrates into the pelvic cavity.
Another reason can be weakened uterine walls secondary to the repeated operation scars. There have been several incidences where doctors have retrieved Mirena from sites others than the uterine cavity (7).
The perforation of the uterus can have drastic consequences. It leads to a condition called ‘acute abdomen’. The contents of uterine cavity irritate the inner-most layer of the abdominal wall called the peritoneum. This leads to peritonitis and a shock-like condition. This is one of the surgical emergencies and requires quick intervention. The procedure usually done is exploratory laparotomy and the primary defect is either closed or uterus is removed in severe instances.
The only way to prevent this potentially life-threatening complication of Mirena is to keep a track of the device’s thread. If you feel that you cannot locate the thread of the device, you should consult your doctor immediately.
Expulsion
This complication usually follows an improper placement of the device.
The IUD gets expelled and you can’t locate the thread. In such case, you should consult your doctor immediately to see if the missing thread is due to perforation or expulsion of Mirena.
Back pain
Back pain associated with IUD use is a common side effect.
There are lots of causes of back pain ranging from nothing significant to something serious.
Some women using Mirena suffered from persistent back pain which was caused by Mirena migration in the pelvic or abdominal cavity (15).
So be careful if you suffer from a persistent back pain while using Mirena and always seek an immediate medical attention in such case.
Ovarian cysts
Mirena is a hormone-releasing device. While its effects are largely local, that is, limited to the uterus, it also has a number of effects on the body as well.
One such effect can be hormonal change leading to the over activity of ovaries, which may result in ovarian cyst formation.
In one research, scientists compared the incidence of ovarian cyst formation in females using Mirena vs females who had undergone hysterectomy. The study included 236 females divided into two groups (Mirena users and hysterectomy group).
At the beginning of the study Mirena users had 12 ovarian cysts compared to 4 ovarian cysts in the hysterectomy group.
Over 12 years Mirena group patients had on average 14 new ovarian cysts while hysterectomy group patients only had 8 new cysts (16).
However, the good news is that more than 94% of these cysts are functional and resolve spontaneously on their own.
Still, you should get regular ovary function checkups while using Mirena or any other hormonal IUD device.
Infection
Although Mirena is made of non harmful materials it is still a foreign element inside your body.
That’s why it acts as a perfect breeding ground for infection causing bacteria.
In severe cases, the use of intrauterine devices like Mirena can lead to a complication called the Pelvic Inflammatory Disease (PID) (16).
PID is a condition caused by overgrowth of infection causing bacteria or fungi in your reproductive track.
This can lead to inflammation of uterus, fallopian tubes, and ovaries.
Most common symptoms of PID include:
- Painful menses
- Pain during intercourse
- Lower abdominal pain
- Fever
- Smelly vaginal discharge
- Infertility
So beware of any abnormal vaginal discharge while using any intrauterine device.
This could be the first sign of PID.
Also, beware of pain during intercourse or menses. Talk to your doctor immediately if you experience any of these symptoms.
Breast tenderness
Some women also complain of breast tenderness while using hormone based IUDs such as Mirena. The pain can be cyclic or can be continuous. Tell your doctor about this problem and ask him/her for help or proper examination. It may be totally harmless but also a sign of something more serious (e.g. breast cancer).
Breast cancer
This is probably one of the biggest concern and one of the most controversial issues related to Mirena use.
In one cohort study, the scientists studied the role of Levonorgestrel-releasing intrauterine systems (LNG-IUD) in the development of breast cancer.
Out of 93 485 women, around 2015 women developed breast cancer, predominantly lobular carcinoma of the breast.
Levonorgestrel-releasing intrauterine systems (such as Mirena) were actually identified as one of the biggest risk factors for breast cancer development (18).
Therefore, it is extremely important that you get regular breast examinations if you use Mirena as your contraception method.
Infertility
Mirena mostly affects endometrium (the innermost layer of the uterus) and has very little hormonal effects on other parts of reproductive system.
In one research scientists studied the effects of LNG-IUDs (such as Mirena) on fertility.
After LNG-UID removal, almost 86% of females gave birth to live babies within 24 months and no permanent infertility was reported (19).
However, there is still a small risk of infertility associated with Mirena use.
Another factor that could make you prone to becoming infertile is infection (PID).
Other documented side effects associated with Mirena use
Use of LNG-IUDs can lead to an increase of hormonal levels in the body.
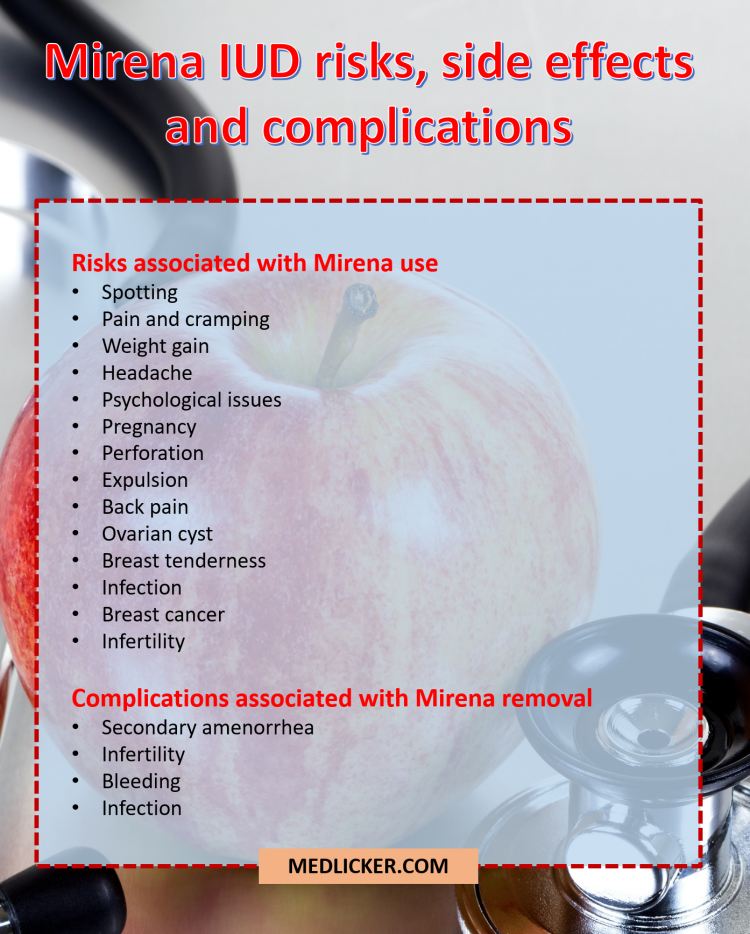
Overview of side effects, risks and complications associated with Mirena IUD
This can lead to an imbalance of sex hormones in the body, which may result in lack of libido or acne outburst (21).
Risks and complications associated with Mirena removal
The main side effects associated with LNG-IUDs removal are as follows:
Secondary amenorrhea
While Mirena removal is quite easy there have been reports of some complications associated with this procedure.
Some practitioners left the hormonally active part of LNG-IUD coil in the uterus, which led to complications like secondary amenorrhea and infertility (20).
Therefore make sure you select your doctor properly and make sure he/she removes Mirena completely to avoid this issue.
Bleeding
As your practitioner is removing the IUD, it brushes against the border of your uterus, cervix and vagina.
So it is quite normal to experience some slight bleeding after LNG-IUD removal.
You might bleed for a couple of days following Mirena removal.
However in case of Mirena heavy post-removal bleeding you should consult your doctor immediately.
Infertility
The fertility returns quite quickly following Mirena removal.
As mentioned above, most of the females recover to their pre-IUD fertility levels witin 12-24 months.
However a very small amount of women may experience an extended period of infertility.
This may be secondary to uterine infection or retention of the hormonally active part of the device.
In such case it is necessary to consult your doctor immediately.
Infection
Infection is a side effect associated with both IUD use and removal.
Signs of infection associated with Mirena removal may be painful periods, pain during intercourse, fever or abdominal pain.
In such case seek immediate medical attention.
Things to remember
Mirena is one of the safest LNG-IUDs on the market.
It is both effective and generally safe to use.
However, you may experience some side effects associated with both Mirena use and removal.
Some of the side effects include spotting, infection, ectopic pregnancy and a slight increase of breast cancer risk.
Post removal complications include bleeding and infection.
Talk to your doctor about any concerns or questions you may have about Mirena use and adverse effects.
| Written by: | Michal Vilímovský (EN) |
|---|---|
| Education: | Physician |
| Article resources: | See numbered references within the article. |
| Image resources: | Adobe Stock |
| Published: | January 25, 2017 at 7:30 PM |
| Next scheduled update: | January 25, 2019 at 7:30 PM |
Get more articles like this in your inbox
Sign up for our daily mail and get the best evidence based health, nutrition and beauty articles on the web.

Ache in left arm that you should not ignore
Alkaline water dangers: why you should not drink it
How to Avoid Sleepiness While Studying?
23 Foods That Increase Leptin Sensitivity
Low dopamine (e.g. dopamine deficiency): causes, symptoms, diagnosis and treatment options
Swollen taste buds: the ultimate guide to causes, symptoms and treatment
Thin endometrial lining: causes, symptoms, diagnosis and treatment
Pimples inside nose: the complete guide
Holes in tonsils: definition, symptoms, treatment and prevention
How to deal with an ingrown hair cyst
Allegra vs. Zyrtec vs. Claritin
How to get rid of phlegm (excessive mucus) in throat? Detailed guide to medical and home remedies, symptoms and causes
Allergy to penicillin and alternative antibiotics
What causes stomach ache after meals?
Liver blood test results explained