Benign esophageal stricture: causes, symptoms, diagnosis and treatment
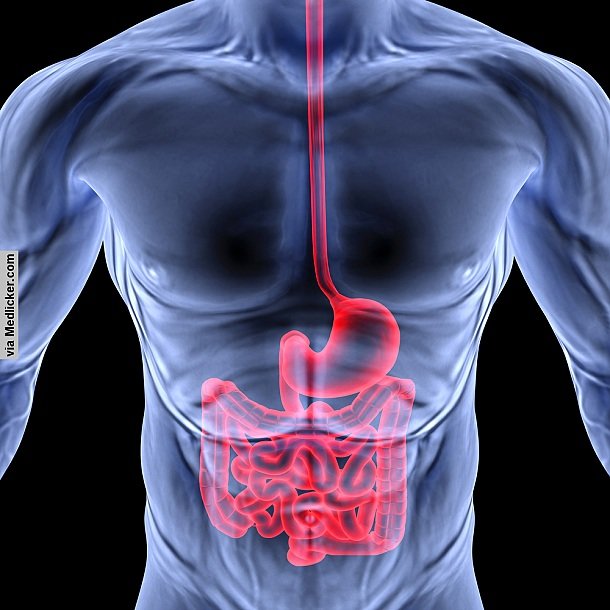
What is meant by benign esophageal stricture? Benign esophageal stricture is narrowing or tightening of the esophagus. In other words, it is a condition in which the diameter of the esophagus becomes narrow. Esophagus is a muscular tube that connects the throat to the stomach and transports food to the stomach. It is about 8 inches long and is lined by pink moist tissue called mucosa. The word benign means that the condition is cancerous yet harmless and it can’t spread to other parts of the body.
Benign esophageal stricture causes difficulties in swallowing food, saliva or liquids and increases the risk of choking. It impairs the passage of food or liquid through the esophagus with a sensation of fullness or pressure in the chest. This condition lasts for a short time in most cases, but in rare conditions, it may be prolonged demanding emergency intervention.
What are the causes of benign esophageal stricture?
Gastroesophageal reflux disease
Gastroesophageal reflux disease (GERD) is a condition that affects the lower esophageal sphincter. Lower esophageal sphincter is a ring of muscle present between the esophagus and stomach. In normal digestion, it opens when food has to be passed from the esophagus to the stomach and after it has delivered the food it closes to prevent the back flow of the food particles and stomach acids from the stomach to the esophagus.
In GERD this sphincter is either weak or relaxes inappropriately due to which return of the stomach contents into the esophagus starts. GERD is the most common cause of esophageal strictures. It is the cause in 70-80% of the cases. This disease is more common in men above 40 years of age, but can occur in any sex or age group.
Excessive acid reflux from the stomach results in inflammation of the lower part of the esophagus, creating heartburn or a burning sensation in the chest. Repeated exposure to harmful stomach acid increases injury and inflammation. This ultimately leads to healing, but when this whole process continues for a long time it causes scarring of the esophagus. Eventually, a benign stricture develops that narrows the opening of the esophagus.
Ingestion of corrosives
Corrosives are another cause of the esophageal sphincter stricture. Corrosives are substances that can attack and destroy exposed body tissues. They can cause damage to the body tissues as soon as they come into contact with them.
Common corrosives are hydrochloric acid, nitric acid, sulfuric acid, chromic acid, hydrofluoric acid, acetic acid, ammonium hydroxide, potassium hydroxide and sodium hydroxide. When corrosives are swallowed, they cause damage to the lining of the esophagus, mouth, throat and stomach. Due to corrosive damage, scarring develops that cause stiffness of the esophageal lining. The result is narrowing of the esophageal sphincter and swallowing problems.
Extended use of a nasogastric tube
Extended use of nasogastric tube can lead to esophageal stricture. Nasogastric tube is a tube that carries food and other materials from the nose to the stomach. It is mainly used in patients that are usable to swallow food and liquids on their own. When this tube is passed again and again or used for a long time, it can cause inflammation of esophagus and scarring. This leads to constriction of the esophagus with symptoms of difficulty in swallowing and food regurgitation.
Esophageal rings
Esophageal rings can cause narrowing of the esophagus. A concentric, thin and smooth extension of normal esophageal tissue is called as an esophageal ring. It is usually 3-5mm in diameter. It consists of all 3 anatomic layers; mucosal, sub mucosal and muscle layer. This ring can be present anywhere along the esophagus, but usually it is present in the distal part of the esophagus.
Esophageal rings are of three types, classified as A, B, and C. Type A ring is uncommon.
This muscular ring is present 1.5 centimeters proximal to the squamocolumnar junction (the point where the epithelium of the esophagus changes from the squamous to columnar). This ring is not fixed and is rarely symptomatic. Type B ring is the most common in the esophagus also known as Schatzki ring.
It is composed of mucosa and submucosa only. It is located at the junction between the esophagus and the stomach and can be present for years. It is non-progressive. Schatzki ring can be seen after swallowing of a solution of barium dye which is visible on X-rays and taking out X-rays of the esophagus. This non-cancerous ring causes swallowing problems (dysphagia). It can be easily treated with dilation of the esophageal stricture by the passage of a dilator. Type C ring is a rare. It can be found incidentally on X-ray and rarely causes symptoms. It is caused by the diaphragmatic crura.
Other causes
Damage caused by an endoscope
Endoscope is a lighted, thin tube that is used to see inside the body in the form of images for evaluation or diagnosis. This tube is passed through the mouth into internal body. Sometimes it may cause esophagitis (inflammation of the esophagus) leading to esophageal strictures.
Treatment of esophageal varices
Esophageal varices are enlarged veins in the esophagus usually in the lower part that can bleed. These are often treated with endoscope which can cause post operative esophageal constriction.
Hiatal hernia
Hiatal hernia is a condition in which stomach bulges up into the thorax through the diaphragm. It is strongly associated with a gastric esophageal reflux disease which then leads to scarring and narrowing of the esophagus.
Postoperative strictures
In about 10% of people esophageal stricture is a complication of the previous surgery. After surgical treatment of esophageal atresia (obliteration of lumen) or any other esophageal operation, esophageal constriction can occur. This is known as postoperative esophageal strictures.
Drug related stricture
Some studies have shown that drugs like non-steroidal anti inflammatory drugs or NSAIDs, iron and alendronate can cause esophageal strictures in some people.
Congenital esophageal stricture
Benign esophageal strictures can be congenital (existing at or dating from birth) in origin. Membranous diaphragm is a congenital problem that may lead to esophageal stricture.
Achalasia
Achalasia is a gradual thickening of the muscles present in the lower end of the esophagus. This thickening disturbs the normal functioning of the lower esophageal hisphincter, which in turn leads to constriction of the esophagus.
What are the risk factors of benign esophageal stricture?
Gastric esophageal reflux diseases
Presence of this disease increases the risk for the development of corrosive scarring and leads to stricture formation.
Swallowing of substances that damage the lining of the esophagus, such as lye, household cleaners, disc batteries, or battery acid can also lead to scarring and narrowing of esophagus.
Esophageal diverticula
Diverticulum is a pouch or sac originating from a tube like organ, such as esophagus. It protrudes into the weak portion of the lining of the esophagus. Usually this condition is asymptomatic but it may become symptomatic.
Dysphagia (difficulty in swallowing), aspiration (collection of fluid) in the lungs and regurgitation (back flow) of food are the main symptoms.
Esophageal stenosis
Stenosis is one of the greatest risk factors for esophageal strictures. Narrowing of the esophagus occurs in this condition. When it persists for a long time it leads to inflammation. Long term inflammation may cause scarring and increases the likelihood of developing stricture.
NSAIDs
These drugs should be avoided in patients of GERD. When a patient with a disease is given these medicines chances of benign stricture formation increases many folds.
Surgery
Esophageal surgeries can cause weakness of the esophagus. Rarely, scar tissue can develop and disturb the functioning of sphincter muscles which then leads to contriction.
Other risk factors
Radiation therapy, sclerotherapy on the esophagus, antibiotics, scleroderma, esophagitis and infectious skin diseases are the other risk factors.
What are the signs and symptoms of benign esophageal stricture?
Signs and symptoms include:
- Heartburn
- Bitter or acid taste in mouth
- Choking
- Cough
- Shortness of breath
- Frequent burping or hiccups
- Pain or trouble with swallowing
- Throwing up blood
- Unintentional weight loss
- Regurgitation of food or liquid: Regurgitation is backflow of substances from the stomach to esophagus or mouth. Sometimes, food may be aspirated into the lungs. Symptoms of aspiration are shortness of breath, cough and wheezing.
- Dysphagia: It is defined as difficulty in swallowing food and liquids or feeling that food is not normally passing into the stomach.
- Feeling of fullness in the chest
- Pressure like sensations in the chest
- Chest pain after meals
- Shortness of breath
- Increased salivation
- Dehydration
How to diagnose benign esophageal stricture
A medical history and physical examination
When you go to your doctor he will ask about all your symptoms and will take a detailed medical history. He will seek your permission for a physical exam. If he will suspect any serious problem, he will refer you to a specialist of the gastrointestinal tract (gastroenterologist) who will examine your gastrointestinal system. He will rule out any malignancy. Then he will ask for some special tests to confirm diagnosis.
Barium swallow
Barium swallow is an X-ray of throat and esophagus. It is also called as barium esophragm. Before starting this X-ray you will be given thick liquid called barium to drink. The barium will temporarily coat the linings of the throat and esophagus and it will help to show up sharp, clear and better images of the gastrointestinal track on the X-ray. In this test a series of esophageal X-rays are taken during and after barium swallow. It is the appropriate method of diagnosis and shows narrowing of the esophagus in esophageal stricture. This test can also be performed before endoscopy is arranged and is usually preferred when urgent confirmation of the diagnosis is needed.
CT scan
Computerized tomography is a technology that uses computer-processed X-rays to produce topographical images of specific areas of the object that allows one to see what is inside of the body without cutting or opening it. CT-scan is useful mainly in malignant conditions, but it is also performed in benign esophageal stricture to rule the malignancy and confirm that it is non-cancerous condition.
Upper gastrointestinal endoscopy
Endoscopy means looking inside. It refers to looking inside the body with the help of endoscope for medical investigation. An endoscope is an instrument which is used to examine or view the interior of a hollow organ or cavity of the body by directly inserting it into the organ. Endoscope is a flexible tube to which light and camera are attached to its one end. It is passed under local anesthesia. It shows narrowing of the esophagus and also helps in finding out the cause. There are disadvantages of endoscopy too. It may delineate the lesion. There is a risk of perforation or a tear in the stomach or esophagus lining. Bleeding can occur and sometimes it may even cause stricture formation by narrowing down the esophagus.
Biopsy
The last option in diagnosis is a biopsy of the stricture. Endoscopy also allows the biopsy of the lesion. Biopsy helps in determining the cause, but this test is usually performed only in malignant conditions.
Esophageal pH monitoring
This test measures the pH of the esophagus. Usually pH is more in the esophagus as compared to stomach. When backflow of the stomach acid into the esophagus occurs its pH falls. To perform this test a tube is inserted from the mouth to the esophagus, which measures pH and amount of stomach acids in the esophagus over a period of 24 hours.
Esophageal manometry
It measures the tone in lower esophageal sphincter. Decreased tone and impaired motility detected by this technique are diagnostic of benign esophageal stricture. Esophageal manometry may not be possible with tight strictures.
Treatment of benign esophageal stricture
Followings are the treatment options:
Diet and lifestyle changes
Dietary and lifestyle changes are effective in managing esophageal strictures. Followings are recommended in patients of benign esophageal strictures:
- Raise the edge of your bed or use high pillows under your head. Elevation reduces the back flow of stomach contents into the esophagus.
- Avoid food intake just before sleep. Don’t eat anything for at least one or two hours before bedtimes.
- Stop smoking. Smoking can adversely affect your gastrointestinal tract and can increase the chances of this condition.
- Avoid alcohol, as it can also upset your gut and can increase acid reflux.
- Use fruits, drinks and soft food so that they can be swallowed easily and without pain. Avoid hard foods, these can damage your throat and increase dysphagia. Till dysphagia is managed avoid them.
- Avoid swallowing corrosive substances. Observe safety measures before coming into contact with such chemicals.
- Instead of large, heavy meals take small and divided meals.
- Avoid tight clothes.
- Some foods increase reflux to the esophagus. Avoid these foods. These include fatty foods, spicy foods, chocolates, carbonated beverages, colas, substances containing caffeine, coffee, citrus products and tomato products.
- Try to lose some weight.
- Improve your oral health.
Esophageal dilation
The best option for the treatment of benign esophageal stricture is esophageal dilatation. This procedure is usually performed at the same time when upper endoscopy is done. With the help of endoscope interior of the esophagus is viewed and if narrowing or benign stricture is found it can be dilated. There are many ways to dilate esophagus.
In one method a balloon dilator also known as boogie is passed with the aid of endoscope, and then this balloon is inflated within limits of the stricture to stretch the esophagus. This process is usually performed under local or general anesthesia, spray or mild sedative for comfort and pain free procedure. Instead of passing dilator through the endoscope it can be passed alone as well. This gives the same results.
Other types of dilators can also be passed during endoscopy. These include mallony and savory dilators. These are used in accordance with the size of a stricture. For smaller stricture mallony dilator is used while savory dilator is used for a large size stricture. There is a need to repeat the esophageal dilation after a period of time in order to prevent the esophageal stricture from narrowing again. Frequency of repetition of this method can be reduced by the use of proton pump inhibitors for a long time.
Some risks are associated with esophageal dilation. These include infections, tear, potential bleeding and perforations. Weight loss and heartburn are the most frequent problems seen in many patients after dilation.
Esophageal stent placement
Esophageal stents are an effective method of treating esophageal strictures. Insertion of stents can provide long term relief of stricture. A stent is a thin tube made of plastic, metal or other material. Local anesthesia should be given before this procedure to numb the throat and esophagus.
Different types of esophageal stents are available. They vary in length and range from 60-150 millimeters. Upper endoscopy is used to guide stent placement exactly at the site of the stricture.
Procedure of implantation of stent is very simple. After placement of a stent its proper positioning can be confirmed by X-ray. The length and diameter of the stricture are first measured, and then a stent is selected usually 1 to 2 centimeters larger than the stricture to avoid in folding of the ends. Complications of the esophageal stent placement are esophageal perforation and stent migration (the stent can move or displace from its original place). Erosion of surrounding tissues of the stent can occur with the use of permanent stents. Tumors can also grow in the stent.
Medications
Proton pump inhibitors
Proton pump inhibitors (PPIs) are the drugs which are used to control excessive gastric acid levels. They are inhibitors of acid secretion. These drugs are very effective for the management of GERD as well as for those conditions in which backflow of the stomach acid to the esophagus causes damage to the esophagus.
These drugs block the proton pump, which are necessary for the release of stomach acids. When these proton pumps are blocked there is less release of gastric acids.
Short term course or long term course of these drugs is prescribed by the doctor according to your condition to provide you relief and prevent recurrence. PPIs include omeprazole, pantoprazole, lansoprazole and esomeprazole.
Adverse effects of these drugs when they are used for short term are headache, fatigue, nausea, diarrhea and dizziness. Long term side effects are vitamin B12 deficiency, rash, constipation, itch, anxiety, flatulence, depression, erythema, constipation, acute interstitial nephritis and pancreatitis.
H2 antagonists
H2 antagonists are drugs that block the action of histamine (a chemical involved in the regulation of the functions of the gut and local immune responses) on the parietal cells in the stomach. The effect of these drugs is decreased production of the acid by these cells. Cimetidine and ramitidine belong to this group.
Ramitidine is the drug of choice from H2 antagonists for the treatment of esophageal stricture. When acid production is decreased there is less backflow of the stomach acids into the esophagus so there is less inflammation, less scarring and less damage.
Side effects of H2 antagonists are known as adverse drug reactions (ADR).
Frequent ADR is hypotension.
Less common ADR are headache, tiredness, dizziness, confusion, diarrhea, constipation, and rash. Cimetidine gives severe adverse effects like hypotension, gynecomastia, impotence and loss of libido.
Surgical treatment
Usually surgery is not recommended for benign esophageal stricture but if your symptoms have not improved by the use of esophageal dilators or medications then you may need it. If the strictures are too wide then your doctors might go for surgical treatment. Anti-reflux procedures are one of surgical operations for treatment. These include Collis-Nissen or complete fundoplication and Belsey or partial gastroplasty. Esophageal resection is another surgical option in which esophagus can be replaced with either stomach, colon or jejunum.
Complications of bening esophageal stricture
Benign esophageal stricture can cause some complications. Commonly seen complications are described below.
- Food may get stuck in the esophagus causing complete obstruction. Drinking of water and other maneuvers fail to dislodge this obstruction. It is an emergency condition and demands immediate correction. Endoscopy can be used to relieve this complication.
- Malnutrition can occur. As esophageal stricture is associated with difficult and painful swallowing. It may hinder one from food intake. One may completely avoid food to get over dysphagia. This can lead to severe nutritional deficiency called as malnutrition.
- Aspiration pneumonia is the most serious complication that can occur. It occurs due to aspiration of the food in the lungs. Aspiration pneumonia gives symptoms of wheezing, shortness of breath and cough.
| Written by: | Michal Vilímovský (EN) |
|---|---|
| Education: | Physician |
| Published: | May 15, 2014 at 4:32 AM |
| Next scheduled update: | May 15, 2016 at 4:32 AM |
Get more articles like this in your inbox
Sign up for our daily mail and get the best evidence based health, nutrition and beauty articles on the web.

Ache in left arm that you should not ignore
Alkaline water dangers: why you should not drink it
How to Avoid Sleepiness While Studying?
23 Foods That Increase Leptin Sensitivity
Low dopamine (e.g. dopamine deficiency): causes, symptoms, diagnosis and treatment options
Swollen taste buds: the ultimate guide to causes, symptoms and treatment
Thin endometrial lining: causes, symptoms, diagnosis and treatment
Pimples inside nose: the complete guide
Holes in tonsils: definition, symptoms, treatment and prevention
How to deal with an ingrown hair cyst
Allegra vs. Zyrtec vs. Claritin
How to get rid of phlegm (excessive mucus) in throat? Detailed guide to medical and home remedies, symptoms and causes
Allergy to penicillin and alternative antibiotics
What causes stomach ache after meals?
Liver blood test results explained