Leishmaniasis: causes, symptoms, diagnosis and treatment
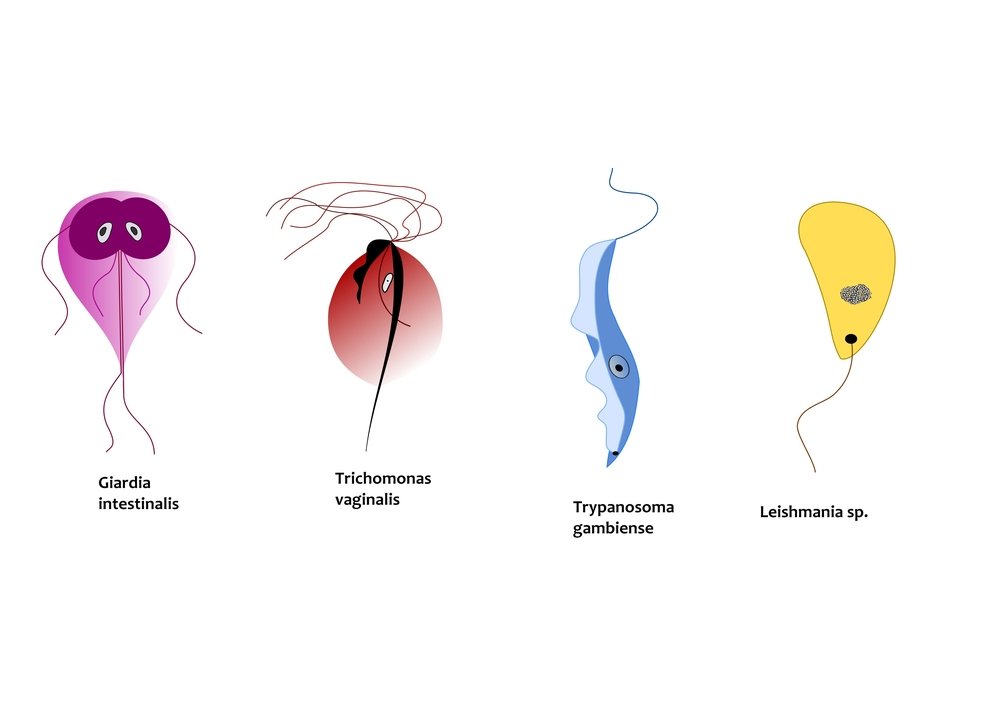
Leishmaniasis is a disease caused by the parasites inside human body. These parasites are Protozoans and belong to the genus Leishmania
The disease is further divided into three types:
- Cutaneous Leishmaniasis: It is the most common form and involves external Skin of the Human Body.
- Mucocutaneous Leishmaniasis: This type commonly affects Nose and Mouth and other mucosal surfaces along with the external Skin.
- Visceral Leishmaniasis: It is a severe form of disease. It involves infection of Internal Organs as well as Skin. It is also known as kala-azar.
All these forms differ in site of infection and symptoms which appear. It also affects other animals other than humans, for example dogs, cats, rodents etc. Leishmaniasis affects about 2 million people each year, and causes almost 20 to 50 thousand deaths. At present about 12 million people in the world are suffering from Leishmaniasis.
Causes of Leishmaniasis
Infectious agent of the Leishmaniasis is a Protozoan Parasite. This parasite can be any one out of the 20 species of the genus Leishmania.
Vector: This infective parasite is transferred to humans by the bite of infected Phlebotomine Sandflies.
Mechanism of infection along with life cycle of the parasite is as follows:
- Sandflies that are infected, when take blood meal from host (Human), transfer the parasite in its Metacyclic Promastigote form.
- Metacyclic Promastigote at puncture site is phagocytosed by the Macrophages.
- Inside Macrophages they are transformed into the Amastigote form.
- Amastigote form of the parasite is infective to humans and multiplies in the affected tissues. Type of tissue in which they divide depends to some extent on the species of the parasite.
- Disease manifests itself in form of particular symptoms according to the tissue type involved. Hence infection of specific tissues causes a specific type of disease.
- When a Sandfly bites an infected host for blood meal it takes up the parasite in Amastigote form present in the blood.
- Amastigote form reaches the gut of the Sandfly and differentiates into Promastigote form.
- Promastigote form further divides and changes to Metacyclic Promastigote form. In this stage parasite travels upwards and reaches the elongated mouth (Proboscis) of the Sandfly. Parasite at this stage is ready to infect next host as Sandfly bites another person for blood meal.
Disease Types
Visceral Leishmaniasis is caused by three species of genus Leishmania. These are Leishmania donovani, Leishmania infantum and Leishmania Chagasi. Cutaneous and Mucocutaneous Leishmaniasis can be caused by all of 20 Leishmania species.
Risk Factors
People with poverty and malnutrition, and those living in areas where urbanization and deforestation has taken place, are at an increased risk of getting infected with Leishmania.
Symptoms of Leishmaniasis
Leishmaniasis is associated with specific symptoms according to type of the disease involved. Common symptom however is formation of skin sores. These sores are formed weeks to months after the bite of the infected Sandfly.
Specific symptoms which appear in its 3 types are as follows:
- Cutaneous Leishmaniasis: Symptoms of the Cutaneous Leishmaniasis include Skin sores at the site of Sandfly bite. This sore appears weeks to months after bite and usually heals on its own. It takes about few months to a year and half to heal. However it leaves behind unpleasant looking scar. In severe diffused form of the disease sores are widespread on the body and do not heal on their own. These lesions usually resemble those of Leprosy.
- Mucocutaneous Leishmaniasis: In this form lesions appear on skin as well as mucosal surfaces. Most common mucosal surfaces involved are nose and mouth. Ulcers are formed at these parts of the body along with external skin sores.
- Visceral Leishmaniasis: It manifest as skin sores initially. However months to years later after initial infection other more serious symptoms start to appear. These include Anemia, Fever, damage to Liver and Spleen etc. Enlargement of Spleen can be remarkable in Leishmaniasis.
Examination and diagnosis of leishmaniasis
Diagnosis of Leishmaniasis is based on history of patient certain clinical examination procedures and specific laboratory tests.
History: On taking history patient will tell about being in an area of infected people or where the disease is common. History will also indicate that patient was bitten previously by a Sandfly.
Examination: Patient on physical examination will show signs of Leishmaniasis. These may include enlargement of Liver and Spleen. Swollen Lymph Nodes may also be present. Skin sores at site of Sandfly bite or elsewhere on body are common in all forms of the disease. However in Visceral Leishmaniasis patient will have Anemia, Fever, Weight Loss, thinning of the Hair and Abdominal discomfort etc.
Laboratory Tests: Laboratory Tests are most important in exact diagnosis of the disease.
- Classic test for diagnosis is Culturing. Biopsy is taken from the area which is affected. It can be Skin, Liver, Lymph Node or Spleen. Then this biopsy is grown by providing suitable conditions to the Parasite. Identification of the Parasite in the grown culture is confirmatory. Slides can be prepared from the biopsy taken as mentioned above or from the peripheral Blood. These slides are stained with Leishman’s stain to colour the Organism. Now the stained slides are observed under the microscope. Parasite is mostly found in Amastigote form around Monocytes and Neutrophils in Blood specimen. In Biopsy specimen these are found near Macrophages. Despite the accuracy, taking specimen from the lesions is a painful procedure for the patient. And it also requires highly trained and experienced personnel to identify the infected cells.
- New easy techniques have been developed which are readily available and easy to perform for the diagnosis of Leishmaniasis. These are Immunological in nature and are based on identifying antigens or antibodies present in body related to the Parasite. Parasite has specific molecules on its surface which help in its identification by Immune System as foreign harmful particle and produce specific response. These molecules are called Antigens. Immune System in response to these antigens produces Antibodies which are molecules that attach to this Antigen and form Antigen-Antibody complex. Both these particles can be identified and form the basis of these Immunological Tests. Immunological Tests include :
- Enzyme-Linked Immunosorbent Assay (ELISA)
- Antigen Coated Dipsticks
- Direct Agglutination Test (DAT) However, these tests lack both Sensitivity and Specificity.
- A new very Specific and Sensitive test for diagnosing Leishmaniasis is PCR (Polymerase Chain Reaction) test. In this test, DNA of the Parasite is multiplied in laboratory and then identified by machines. It gives very accurate results, however it can be expensive.
- If further analysis is required for research purposes, species can also be identified by Isozyme Analysis and DNA sequencing.
Treatment of Leishmaniasis
There are certain drugs available for the treatment of Leishmaniasis. These include:
- Antimony containing Drugs (Meglumine Antimoniate, Sodium Stibogluconate)
- Amphotericin B
- Paromomycin
- Pentamidine
- Ketoconazole
- Miltefosine Drug and course of treatment vary according to the Geological location of the patient, Species involved and type of the infection.
In India, Visceral Leishmaniasis is resistant to the Antimony Drugs. Hence treated with liposomal Amphotericin B. Amphotericin B is also used in South America and Mediterranean region for Visceral Leishmaniasis.
In Africa, Antimony Drugs combined with Paromomycin are given. Miltefosine is effective drug for Visceral as well as Cutaneous Leishmaniasis. Cutaneous Leishmaniasis treatment is done infrequently. It is treated with certain drugs which are specific for specific Species of Leishmania.
Topical Paromomycin is effective against Leishmania major, Leishmania tropica, Leishmania mexicana, Leishmania panamensis and Leishmania braziliensis. Pentamidine is given for Leishmania guyanensis. Leishmania tropica and Leishmania major can also be treated by oral Ketoconazole, Fluconazole and Itraconazole. Despite these drugs, disfigurement caused by skin sores, especially on face, requires Plastic Surgery.
Treatment of Leishmaniasis on Community scale requires its prevention and elimination of Vector. Hence, people of the infected and high risk areas are asked to sleep in beds covered with insect net. Use of lotions and sprays which are insect repellent is encouraged. Insecticide spray on a large scale and on the habitat of the Sandfly is effective in decreasing its population. Infected patients are properly managed to net let them be bitten again by Sandflies as it may produce increased number of Infective Vectors.
Prognosis of Leishmaniasis
If treated properly cure rates are very high in Leishmaniasis. Visceral Leishmaniasis cure rate with single dose of Amphotericin B is around 95 percent. Treatment should be done as early as possible to avoid damage to Immune System and disfigurement of the Body. Skin sores and ulcers caused by Cutaneous Leishmaniasis form disfiguring scars which are permanent and require Plastic Surgery.
If not treated Leishmaniasis (mostly Visceral Leishmaniasis) can cause death. Death occurs in about 2 years after infection. Death is not due to disease itself but because of complications arising from it. Drugs taken during course of therapy may have several side effects. Pregnant women should not take Miltefosine during first three months of the pregnancy as it may cause abnormality in Embryo and Fetus.
Complications of Leishmaniasis
Leishmaniasis can lead to several life threatening complications. Cutaneous Leishmaniasis is associated with:
- Disfigurement of the Body
- Damage to Immune System
- Bleeding Visceral Leishmaniasis produces more severe complications and is often fatal due to the same reason. Complications include:
- Damage to Liver
- Damage to Spleen
- Damage to Immune System
- Bleeding and Fever People with already weak Immune System (AIDS etc.) are at high risk of developing Visceral Leishmaniasis and its complications. Disease is also resistant to drugs mostly in such patients.
| Written by: | Michal Vilímovský (EN) |
|---|---|
| Education: | Physician |
| Published: | April 2, 2014 at 12:35 AM |
| Next scheduled update: | April 2, 2016 at 12:35 AM |
Get more articles like this in your inbox
Sign up for our daily mail and get the best evidence based health, nutrition and beauty articles on the web.

Ache in left arm that you should not ignore
Alkaline water dangers: why you should not drink it
How to Avoid Sleepiness While Studying?
23 Foods That Increase Leptin Sensitivity
Low dopamine (e.g. dopamine deficiency): causes, symptoms, diagnosis and treatment options
Swollen taste buds: the ultimate guide to causes, symptoms and treatment
Thin endometrial lining: causes, symptoms, diagnosis and treatment
Pimples inside nose: the complete guide
Holes in tonsils: definition, symptoms, treatment and prevention
How to deal with an ingrown hair cyst
Allegra vs. Zyrtec vs. Claritin
Allergy to penicillin and alternative antibiotics
How to get rid of phlegm (excessive mucus) in throat? Detailed guide to medical and home remedies, symptoms and causes
What causes stomach ache after meals?
Liver blood test results explained